What is Gingivitis?
Don’t ignore bleeding gums!
Gingivitis is a type of gum disease, caused by the build-up of plaque — a sticky film of bacteria — on the teeth and along the gumline. If not removed through regular brushing, flossing, and professional dental cleans, plaque can irritate and inflame the gums.
The main signs of gingivitis include red, swollen gums that bleed easily when brushing or flossing. In most cases, gingivitis is painless, which means many people don’t realise they have it. Gingivitis is reversible if proper care and maintenance is undertaken. If left untreated, gingivitis can increase your risk of periodontitis, a more serious form of gum disease that may result in tooth loss.

Common Causes of Gingivitis
Gingivitis develops when plaque — a sticky film of bacteria — builds up on the teeth and gums. If not removed by daily brushing, flossing, and professional dental cleans, plaque hardens into tartar (calculus), which irritates the gums and makes it easier for bacteria to thrive. This irritation leads to inflammation, swelling, and bleeding gums.
While poor oral hygiene is the most common cause, several other factors can increase the risk of gingivitis:
Poor oral hygiene habits
- Skipping brushing or flossing allows plaque to accumulate along the gumline.
- Not replacing a worn toothbrush means plaque and bacteria are less effectively removed.
Smoking or tobacco use
- Tobacco reduces blood flow to the gums, making them more vulnerable to infection.
- Smokers are also more likely to have tartar buildup and delayed gum healing.
Hormonal changes
- Pregnancy and menopause can make gums more sensitive and prone to inflammation.
Medical conditions
- Diabetes, certain autoimmune disorders, and diseases that affect the immune system can make it harder for the body to fight off gum infections.
- Viral and fungal infections in the mouth can also contribute to gum irritation.
Poor nutrition
- A diet high in sugar and refined carbohydrates feeds the bacteria that cause plaque.
- Deficiencies in essential vitamins and minerals in the diet can effect gum health and healing.
Ill-fitting dental appliances
- Poorly fitting dentures, bridges, or braces can trap food and plaque around the gums.
Genetics
- Some people are naturally more prone to gum disease due to inherited traits that affect immune response or gum structure.
Symptoms of Gingivitis
Gingivitis is often painless in its early stages, which is why many people don’t realise they have it. Recognising the signs early can help you treat the condition before it develops into more serious gum disease.
Common symptoms of gingivitis include:
Red or swollen gums
Healthy gums should be firm and pink; inflammation changes their colour and texture.
Bleeding gums
Gums that bleed easily when brushing or flossing are a classic warning sign.
Tender or sensitive gums
Discomfort when eating, brushing, or flossing.
Persistent bad breath (halitosis)
Caused by bacteria and plaque buildup.
Receding gums
Gums that start to pull away from the teeth, making them look longer.
Soft gums
Gums may feel puffy or spongy to the touch.
Change in gum shape
Gums may lose their snug fit around the teeth.
Even mild symptoms should not be ignored, as untreated gingivitis can worsen and increase your risk of developing periodontitis.


Treatment of Gingivitis
The good news is that gingivitis is reversible with proper care. Your dentist will first assess the health of your gums and teeth, then create a treatment plan to remove plaque, tartar, and bacteria.
Common treatments include:
Professional dental cleaning
Scaling and polishing to remove plaque and tartar above and below the gumline.
Root planing (deep cleaning)
Cleaning the roots of the teeth to help gums reattach and prevent bacteria from collecting.
Antibacterial rinses or gels
To reduce bacteria and control infection.
Replacing or adjusting dental appliances
Ensuring dentures, bridges, or braces fit properly to avoid trapping plaque.
Treating underlying conditions
Managing health issues like diabetes that can make gums more prone to infection.
Prevention of Gingivitis
Keeping your gums healthy involves a combination of daily care and regular dental visits.
Preventive steps include:
- Brush twice daily with a soft-bristled toothbrush and fluoride toothpaste.
- Floss once a day to remove plaque between teeth and along the gumline.
- Have regular dental check-ups and professional cleans (every 6 months or as recommended).
- Eat a balanced diet rich in vitamins and minerals to support gum health.
- Avoid smoking and tobacco products, which slow gum healing and increase disease risk.
- Manage underlying health conditions such as diabetes.
By combining professional dental care with good home habits, gingivitis can be treated effectively — and even better, prevented altogether.
Contact Dental at Keys to help manage your Gingivitis!
Dental Services
Full Mouth Dental Implants
Dental Implants
Invisalign
Clear Aligners
Cosmetic Dentist
Veneers
Sleep Dentistry
Teeth Whitening
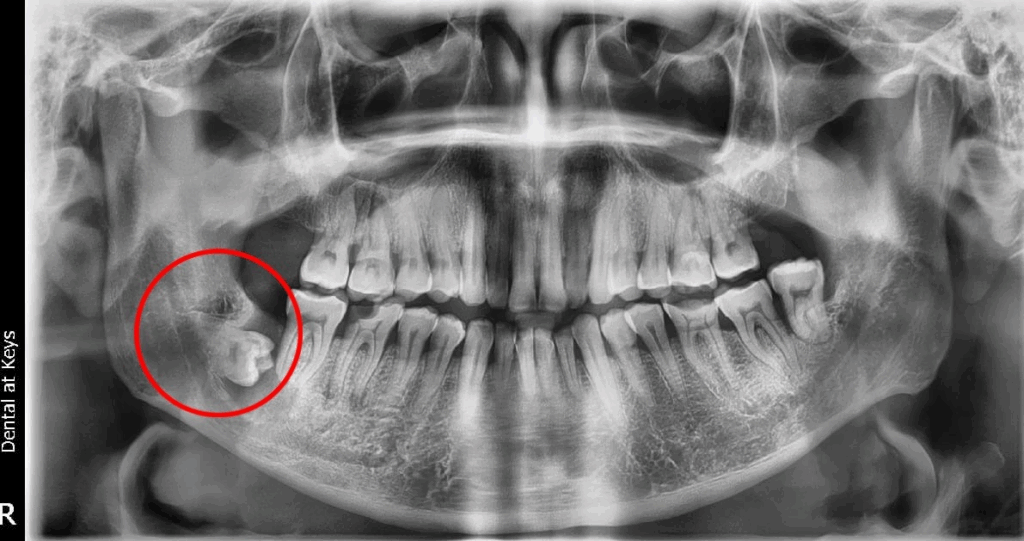
Wisdom Tooth
Orthodontics
Jaw Expansion
Tooth Extraction
Dental Crown
Dental Bridge
Root Canal Treatment
General Dentistry
Gum Disease Treatment
Tooth Filling
Teeth Cleaning
Dentures
Sleep Apnoea
TMJ
Occlusal Splint
Mouth Guard
Family Dental
Kids Dental
Silver Diamine Fluoride
Fissure Sealants
Frequently Asked Questions

Is gingivitis reversible?
Yes, gingivitis is reversible, especially when caught early. With proper oral hygiene, professional dental cleanings, and lifestyle changes, you can eliminate the inflammation and restore your gums to a healthy state. Advanced gum disease – is NOT and hence early detection and treatment is essential.
Can gingivitis lead to tooth loss?
If left untreated, gingivitis can progress to periodontitis, a more severe form of gum disease. Periodontitis damages the bone and tissues that support the teeth, which can ultimately lead to tooth loss. Early treatment of gingivitis can prevent this progression.
Does gingivitis hurt?
Gum disease is usually not painful in its early stages, which is why many people may not realise they have it. However, you may experience gum tenderness, swelling, or discomfort if the condition worsens.
What should I do if I think I have gum disease?
Book an appointment with us as soon as possible because leaving a potential problem is never a good idea.